【www.zhangdahai.com--其他范文】
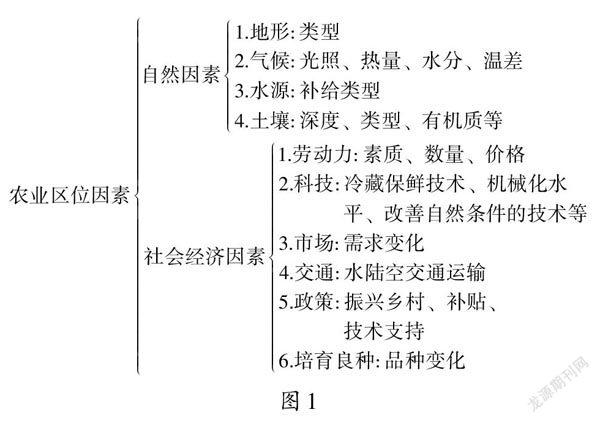
Mei-ning Li, Yan-hui Lu, Ya-min Li, Hai-yun Wang, Yu-hong Mi
Emergency and Critical Care Center, Beijing Anzhen Hospital, Capital Medical University, Beijing Institute of Heart, Lung and Blood Vascular Disease, Beijing 100029, China
Pulmonary thromboembolism (PTE) has become the third most lethal type of thrombotic disease in the world.[1]Thrombolysis has been advised for high-risk PTE patients, however due to its unique pathophysiology,which differs from other atherosclerotic diseases, this can still be a challenge for PTE patients.[2]We reported two cases with a high-risk of PTE that had the onset of or progressed to cardiac arrest (CA) during hospitalization and were successfully managed with cardiopulmonary resuscitation (CPR) combined with thrombolytic therapy.
Case 1
The patient was a 66-year-old man who had come to the emergency department with chest tightness,shortness of breath, and back pain for 15 min. The patient experienced CA when he was transferred to our emergency department three minutes later and received CPR. The patient obtained approximately 10 min of vital sign recovery after CPR, with blood pressure (BP) of 130/75 mmHg (1 mmHg=0.133 kPa), heart rate (HR) of 78 beats/min, and respiratory rate (RR) of 20 breaths/min. An electrocardiogram (ECG) showed marked dilation of the right ventricle and a marked D-shape of the left ventricle (Figure 1). Spontaneous circulation was not restored even after a high dose of vasoconstrictor was administered. Additionally, the patient received a 20 μg/(kg·min) dose of dopamine and a 10 μg/(kg·min)dose of norepinephrine. Pulmonary embolism was highly suspected. However, he had no hypertension, diabetes,or coronary heart disease history. Thrombolytic and tracheal intubation were immediately and simultaneously performed, and subsequently, 50 mg of recombinant tissue plasminogen activator (rt-PA) thrombolytic therapy and endotracheal intubation assisted ventilation were offered. The patient’s vital signs returned to normal within 30 min, and the blood oxygen saturation increased from 0 to 95% as a result of the thrombolytic therapy.
The patient was suspected with PTE and received unfractionated heparin (UFH) for anticoagulant therapy,and the diagnosis of PTE was finally confirmed by computed tomography pulmonary angiography (CTPA)(Figure 2). One day before discharge, his serological biomarkers and blood gas results were within normal ranges: D-dimer 726 ng/mL, cardiac troponin I (cTnI)0.02 ng/mL, pH 7.425, arterial partial pressure of oxygen (PaO2) 61.1 mmHg, arterial partial pressure of carbon dioxide (PaCO2) 39.9 mmHg, and oxygen saturation of blood (SpO2) 98.3%. The patient continued to take warfarin orally for anticoagulant treatment after discharge. He was in stable condition at his oneyear follow-up, and did not complain of any chest tightness, chest pain, or shortness of breath. However,anticoagulation therapy was continued because the patient’s lower extremity vein ultrasound revealed the presence of residual thrombus.
Case 2
The patient was a 62-year-old woman who was hospitalized for dyspnea upon exertion for 2 weeks with edema of the lower limbs and no chest tightness,chest pain, or hemoptysis. Moreover, she had undergone percutaneous coronary intervention for acute myocardial infarction within the past 2 months and had been subsequently immobilized and bedridden for 3 weeks.
Physical examination showed tachycardia (116 beats/min) and hypotension (82/59 mmHg), and her D-dimer was 8,600 ng/mL and cTnI was 0.049 μg/L (normal range<0.023 μg/L). CTPA revealed low-density filling defects in the main lumen of the left and right pulmonary arteries; in the lumen of the left upper pulmonary artery,the lower lobe pulmonary artery and its segmental branches; in the lumen of the right upper pulmonary artery, the middle segment of the right lung artery; and in the lower right pulmonary artery and its segmental branches (Figure 3). Lower extremity deep venous ultrasound revealed that thrombosis occurred in the left inferior segment of the femoral vein bilaterally in the popliteal vein, right posterior tibial vein, and left calf intermuscular vein. Doppler echocardiography revealed tricuspid regurgitation (TRV) of 413 cm/s, a pressure gradient (PG) of 68 mmHg, and systolic pulmonary artery pressure (SPAP) of 83 mmHg. The inner diameter of the inferior vena cava into the right atrial orifice was 20 mm, and the collapse rate with respiration was less than 50% (Figure 4A).
UFH was administered, but her symptoms did not improve. Due to the patient’s double antiplate therapy for myocardial infarction and had high risk of bleeding,inferior vena cava filter implantation and catheterdirected pulmonary thrombosis aspiration therapy were provided following the patient’s admission to the emergency intensive care unit (EICU). The patient’s condition worsened again, and CA appeared within 15 min. Eight minutes of CPR was accompanied by salvage thrombolytic therapy, and 42 mg rt-PA was intravenously administered within 2 h after an 8 mg loading dose through intravenous injection. Two hours later, the patient was restored to a stable condition after thrombolysis with BP of 113/82 mmHg, HR 131 beats/min, RR 25 breaths/min, and SPAP of 41 mmHg (Figure 4B). The endotracheal tube was pulled out 3 days after CPR. UFH combined with warfarin treatment was administered because of severe renal failure, and the patient was discharged after 8-day of hospitalization.The patient’s limbs showed normal muscular strength,and she could walk on the ground without dysphagia,drinking water without coughing, or other sequelae of nervous system function before discharge. In followup treatment, the patient still insisted on oral warfarin anticoagulant therapy due to her age and the existence of high risk factors for thrombosis, such as type 2 diabetes and hyperhomocysteine. Dynamic changes in biomarkers and blood gas analysis are shown in Table 1.

Figure 1. Echocardiogram showing the dilation of the right ventricle and marked D-shaped left ventricle on admission of patient 1.

Figure 2. CTPA revealed multiple bilateral embolisms in the pulmonary artery in the horizontal (A) and sagittal (B) positions for patient 1. CTPA: computed tomography pulmonary angiography.

Figure 3. CTPA revealed multiple bilateral embolisms in the pulmonary artery (A) with enlargement of the right side of the heart (B)in patient 2. CTPA: computed tomography pulmonary angiography.

Figure 4. Echocardiography at the emergency department (A) and 2 h after interventional therapy (B) for patient 2.

Table 1. Dynamic changes in biomarkers and blood gas results from admission to 1 day before discharge of case 2
Cardiac arrest is a cause of death, with an incidence of 28 to 54 per 100,000 people per year.[3]Among all the diseases that cause CA, cardiovascular disease accounts for approximately 70%, and pulmonary embolism accounts for 10%.[4,5]Among patients with massive pulmonary embolism (PE), rates of CA as high as 65%-88% have been reported.[6,7]With an increasing proportion of non-cardiac causes of CA such as PTE,trauma, anaphylaxis, and perioperative conditions,tissue and organ perfusion can be restored, improved,and maintained after timely CPR. However, when PTE patients experience sudden CA, systematic thrombolytic therapy is typically the most practical approach, as was the case with patient 1 and patient 2. After thrombolytic and anticoagulant treatment, the patients’ vital signs recovered, and symptoms of wheezing, chest tightness and dyspnea disappeared. As demonstrated in a previous study,[8]when patients with hemodynamic instability cannot receive CTPA, acute pulmonary embolism should be highly suspected if the patient has abnormal echocardiography, significantly elevated D-dimer, and low oxygen saturation. Thrombolytic therapy should be performed as soon as possible.
Systemic thrombolytic therapy is also suitable for patients who have deteriorated during anticoagulant therapy. Our case 2 developed CA during the application of anticoagulation, which showed that even under close observation during anticoagulant therapy, patients with medium-risk pulmonary embolism can still deteriorate in the acute phase. This case provides information for the observation of signs that might get worse in patients with intermediate risk pulmonary embolism. Since there are many unknown causes of CA, early identification is important for both follow-up and prognosis.
According to the ESC guidelines in 2014,[9]thrombolytic therapy is not recommended as the first choice for PTE patients with stable hemodynamics,but if hemodynamic instability occurs during the acute phase of anticoagulant therapy, rescue thrombolytic therapy should be immediately performed. The results of previous studies have shown that patients with mediumto-high-risk PTE with stable vital signs may develop CA during anticoagulant therapy, and the D-dimer of these patients has been shown to decrease in some cases but increase in others. For patients with elevated D-dimer, it is easy to consider the diagnosis, while for PTE patients with a stable decline in D-dimer during anticoagulation therapy, the occurrence of CA may put clinicians in a passive position, eventually resulting in irreversible outcomes for patients. Therefore, identifying PTE patients who might develop CA during anticoagulant therapy can result in better outcomes.
D-dimer, ultrasonic cardiogram (UCG) and ECG are usually used to monitor the hemodynamics of patients with medium-to-high-risk PTE. When a PTE patient’s D-dimer level increases, it often indicates the imbalanced clot-fibrinolysis system, the uncorrected hypercoagulability and a risk of new thrombosis in the pulmonary artery. The patient in case 1 had an unexplained CA 3 min after admission, and it is necessary to investigate the cause of CA after the CPR were performed and vital signs were recovered.Echocardiography showed an enlarged right ventricle and a marked D-shape of the left ventricle, suggesting a high possibility of acute PE.
However, ECG and UCG may be useful in patients with fibrinolytic dysfunction whose D-dimer levels do not match the thrombotic load. And anticoagulant therapy alone does not prevent the progression of embolism which ultimately leads to CA. ECG with a deeper T-wave in the chest lead during anticoagulant therapy rather than at admission or a typical SIQIIITIII appearance indicate that the patient is deteriorating.[10]
ECG could be used for the early identification of PTE in clinic. When PTE deteriorates, increases in pulmonary vascular resistance (PVR) and mean pulmonary arterial pressure (mPAP) occur that are due to various degrees of blood vessels.[11]Progressive enlargement of the right side of the heart or the presence of a new floating thrombosis on the right side of the heart indicates a worsening condition that can lead to hemodynamic instability. These conditions also result in reduced preload of the left ventricle, which, with a decrease in the left ventricle ejection fraction, leads to a decrease in the amount of blood pumped into circulation throughout the body. This hypotension can eventually lead to obstructive cardiogenic shock. Therefore, early identification of CA and remedial thrombolytic therapy can be crucial for improving the prognoses of patients.
The use of thrombolytic therapy depends on the riskbenefit profile. Although many case reports supported the effectiveness of thrombolytic therapy in highly suspected PE, to our knowledge, no randomized trials have demonstrated the effectiveness of thrombolytic therapy in resuscitation. Studies by Namiranian et al[12]and Ruiz Bailén et al[13]have shown the effectiveness of thrombolytic therapy in patients with clinically suspected PE, and have also suggested the improvements in 24-hour survival, neurological function, and decreased mortality.
Thrombolytic therapy with rt-PA is the first choice for all high-risk PTE in clinic, and it is recommended as standard first-line treatment in patients with massive PTE. According to Zhang et al[14], 50 mg rt-PA thrombolytic therapy was as effective as 100 mg rt-PA in patients with acute PTE, with a significant reduction in bleeding and mortality and no increase in reoccurrence of PTE during follow-up.
The preferred fibrinolytic agent is alteplase infusion as a dose of 50 mg within 2 h, as we used in both of our patients. Only when thrombolytic contraindications exist should pulmonary catheter thrombolysis be considered.It is critical to maintain hemodynamic stability during resuscitation. Here, extracorporeal support can be helpful.
One of the drawbacks of thrombolytic therapy is the potential intracranial and other major bleeding episodes. In a study by Janata et al[15]that included 66 patients with CA secondary to PTE, 25% of them had a fatal bleeding event during thrombolytic therapy, and there was no significantly difference in bleeding complications between patients who had undergone CPR of more than 10 min and those who required less than 10 min of CPR. Other studies presented twelve cases of intracranial hemorrhage in a PTE patient who received thrombolytic therapy, while no intracranial hemorrhage occurred in a PTE patient who did not receive thrombolytic therapy.[16-18]To choose the best course of thrombolysis, the clinician must weigh the benefits to the patient after thrombolysis against the potential disadvantages of bleeding risk.
Accurate diagnosis and quick response are important for managing acute massive PTE. Our cases show that rapidly and effectively administering CPR combined with rescue thrombolysis is feasible for high-risk PTE patients without absolute thrombolysis contraindications. Our cases also show that PTE patients with the occurrence of CA during anticoagulant therapy could also be benefited from rescue thrombolytic therapy.
Funding:This work was supported by the Chaoyang District Science and Technology Commission of China (CYSF2049).
Ethical approval:Study approval was not necessary, as this is a case report, and consent for publication was obtained from the patients.
Conflicts of interest:The authors declare that they have no competing interests.
Contributors:conceptualization: YHL, YHM; data curation:MNL; formal analysis: MNL; investigation, MNL; methodology:MNL, YML; project administration: MNL, HYW; resources:YML; supervision: HYW; writing - original draft: MNL; writing- review & editing: MNL, YHM.
推荐访问:combined thrombolysis resuscitation
本文来源:http://www.zhangdahai.com/shiyongfanwen/qitafanwen/2023/0724/629788.html